Entering your 40s often brings subtle changes in your body that signal the approach of menopause. While these changes can feel unexpected, understanding them early provides a unique opportunity to prepare, manage symptoms, and maintain overall health. How to prepare for menopause in your 40s is more than just a question about hormonal shifts; it’s about adopting a proactive mindset that blends nutrition, lifestyle, emotional awareness, and preventive care.
By recognizing early signs, implementing healthy routines, and exploring safe non-hormonal interventions, women can navigate this transition with confidence. In this article, we’ll break down the physical, emotional, and lifestyle strategies essential for thriving through midlife.
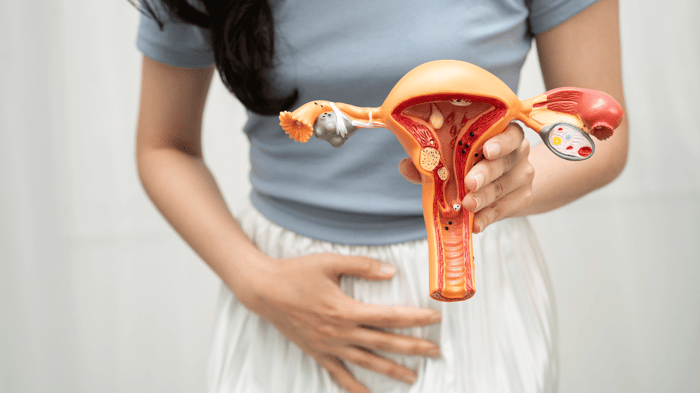
Understanding Perimenopause and Early Signs
Hormonal Shifts in Your 40s
Perimenopause, the transitional phase before menopause, often begins in the early to mid-40s. During this time, estrogen and progesterone levels fluctuate, affecting multiple body systems. Irregular menstrual cycles, hot flashes, and sudden changes in energy are common signals that your body is adapting to new hormonal patterns. These fluctuations can also influence sleep quality, mood, and even sexual health.
Common Symptoms to Watch For
Symptoms of perimenopause are varied and can differ significantly among women. Common early indicators include persistent fatigue, mood swings, vaginal dryness, night sweats, and unexpected weight gain. Tracking these symptoms can help anticipate menopause, making it easier to implement interventions that reduce discomfort and support long-term well-being.
Long-Term Health Implications
Beyond immediate discomfort, perimenopause carries implications for long-term health. Declining estrogen impacts bone density, cardiovascular health, and even cognitive function. By understanding these risks early, women can adopt preventive strategies—like targeted nutrition, exercise, and supplementation—to maintain vitality well into their later years.
Lifestyle Adjustments for Midlife Wellness
Nutrition and Hydration
Eating with menopause in mind can significantly ease symptoms and support hormonal balance. Nutrient-rich foods, including omega-3 fatty acids, leafy greens, and antioxidant-rich fruits, help stabilize mood, reduce inflammation, and protect bone health. Adequate hydration is equally important, as it supports metabolism, skin health, and mucosal moisture.
Exercise Strategies
Maintaining an active lifestyle in your 40s is crucial for heart health, bone strength, and energy levels. Cardiovascular exercise like brisk walking or cycling promotes circulation and cardiovascular wellness. Strength training builds muscle and preserves bone density, while flexibility routines like yoga or Pilates improve balance and reduce injury risk.
Sleep Optimization
Sleep disruption is common in midlife, often caused by hormonal fluctuations or night sweats. Prioritizing quality sleep helps regulate mood, supports cognitive function, and maintains sexual and emotional health. Simple strategies include establishing a consistent sleep schedule, using cooling bedding, and minimizing nighttime light exposure.
Stress Management
Chronic stress can exacerbate menopausal symptoms, from hot flashes to fatigue. Incorporating mindfulness, meditation, and breathing exercises helps reduce stress hormone levels and enhances resilience. Even short daily routines can make a measurable difference in energy and emotional well-being.
Sexual and Vaginal Health
Maintaining Lubrication and Comfort
Vaginal dryness is one of the most common concerns in perimenopause and early menopause. Using water-based or silicone-based lubricants and moisturizers can provide immediate relief. Internal hydration strategies, such as non-hormonal supplements with Slippery Elm Bark or hyaluronic acid, support long-term mucosal health and reduce discomfort during sexual activity.
Intimacy and Libido
Changes in hormones can affect libido, yet maintaining intimacy remains possible. Open communication with your partner about physical discomfort, desires, and expectations is essential. Incorporating regular non-sexual touch, date nights, and shared activities can strengthen emotional connection and maintain sexual satisfaction.
Preventive Healthcare Measures
Routine Screenings
Early perimenopause is an ideal time to schedule preventive screenings. Bone density tests, cholesterol checks, blood pressure monitoring, and mammograms help identify potential health risks before they become significant. Regular check-ups with your gynecologist ensure that changes in sexual health or vaginal comfort are addressed promptly.
Non-Hormonal Supplementation
For women who prefer to avoid hormone therapy, non-hormonal supplements provide a safe and effective way to maintain hydration, tissue integrity, and sexual comfort. Ingredients like Slippery Elm Bark, hyaluronic acid, amino acids, and probiotics support natural lubrication, reduce friction-related irritation, and promote overall vaginal health.
When to Consult a Healthcare Provider
Persistent fatigue, mood changes, severe vaginal dryness, or sexual health concerns warrant professional attention. A gynecologist can assess symptoms, recommend safe interventions, and help design a personalized plan for a comfortable transition through menopause.
Lifestyle Factors – Food, Sleep, and Habits
-
Food as a Sexual Ally: Nutrition can serve as a natural booster for hormonal balance and tissue health. Adaptogenic herbs like ashwagandha can reduce stress and support libido, while polyphenol-rich foods such as berries and dark chocolate improve circulation. Hydration-rich fruits and vegetables maintain mucosal moisture and sustain energy.
-
Sleep Architecture and Libido: Quality sleep underpins physical and emotional readiness for intimacy. Proper rest supports hormonal balance, reduces fatigue, and preserves libido. Simple adjustments, like optimizing the sleep environment and maintaining a consistent bedtime, can enhance overall vitality.
-
Habits That Undermine Connection: Avoiding excessive alcohol and caffeine, quitting smoking, and managing chronic stress all create a foundation for healthy energy, sexual function, and emotional resilience. Addressing these habits ensures your body is primed for both physical and emotional connection.
Frequently Asked Questions (FAQs)
What is the average age for perimenopause and menopause?
Perimenopause usually begins in the early to mid-40s, though some women may experience symptoms earlier or later. Menopause is defined as the absence of menstrual periods for 12 consecutive months, typically occurring between 48–52 years of age.
Can lifestyle changes in your 40s reduce menopausal symptoms later?
Absolutely. Nutrition, exercise, stress management, and sleep optimization can minimize hot flashes, fatigue, and mood swings. Early adoption of these habits supports bone health, cardiovascular function, and overall vitality.
Are non-hormonal supplements effective in midlife?
Yes. Supplements containing Slippery Elm Bark, hyaluronic acid, amino acids, and probiotics have been shown to improve vaginal moisture, reduce discomfort, and maintain tissue integrity without altering hormone levels.
How can I maintain sexual health as menopause approaches?
Open communication, regular non-sexual intimacy, use of lubricants, pelvic floor exercises, and internal hydration supplements can maintain comfort, desire, and satisfaction.
When should I talk to a doctor about early symptoms?
Seek professional guidance for persistent fatigue, severe vaginal dryness, sexual discomfort, or mood disturbances. Early evaluation allows for personalized care and prevents long-term complications.
Taking Charge Before Menopause
Preparing for menopause in your 40s is about embracing a proactive approach. By combining nutrition, exercise, stress management, quality sleep, sexual health strategies, and preventive healthcare, women can enter midlife with confidence, comfort, and vitality.
Recognize early changes, track symptoms, and adopt safe, non-hormonal interventions. Communication with partners, emotional self-care, and regular consultations with healthcare providers create a holistic framework that supports long-term well-being. Taking these steps today ensures that menopause becomes a manageable, even empowering, stage of life.