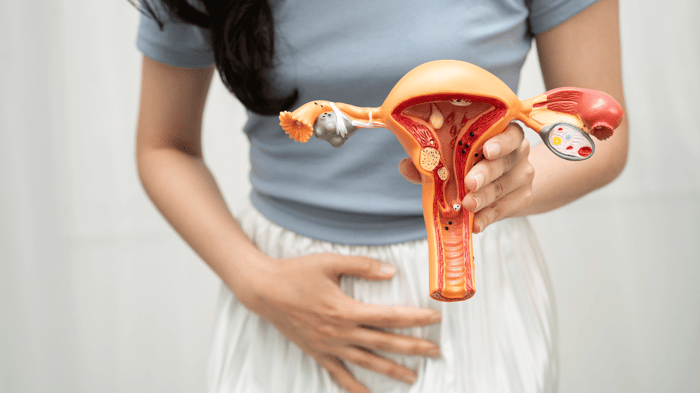
Menopause is a natural and inevitable phase in every woman’s life, typically occurring between the ages of 45 and 55. While it marks the end of menstrual cycles, its effects extend far beyond reproductive changes. One area often overlooked is vaginal health, which can significantly impact comfort, sexual wellness, and overall quality of life.
During menopause, fluctuating hormones—especially the decline in estrogen—can trigger vaginal dryness, thinning of tissues, and other discomforts. Understanding these changes and taking preventive steps is essential for long-term vaginal health. This guide will explore the science behind these changes, non-hormonal strategies to maintain comfort, and emerging tools to support mucosal health.
The Role of Estrogen in Vaginal Health
Why Estrogen is Essential for Vaginal Tissue
Estrogen plays a vital role in maintaining vaginal elasticity, hydration, and microbiome balance. It stimulates blood flow to the vaginal mucosa, keeping tissues plump and flexible, and encourages natural lubrication. Adequate estrogen ensures the vaginal lining remains resilient against friction, irritation, and infection.
When estrogen levels decline during menopause, the vaginal walls can thin, lubrication decreases, and pH balance shifts, creating an environment more susceptible to dryness, discomfort, and infections.
Common Vaginal Changes During Menopause
What Happens to Vaginal Tissue and Secretions
Menopause can trigger several changes in vaginal tissue and secretions:
-
Reduced Lubrication: Lower estrogen results in less natural moisture, leading to dryness.
-
Thinning of Vaginal Walls (Atrophy): The mucosa becomes less elastic and more fragile.
-
Increased Irritation: Friction from everyday activities or sexual activity may cause discomfort.
-
Altered pH Balance: The vaginal environment becomes more alkaline, disrupting the microbiome and increasing susceptibility to infections.
These changes are natural but can affect both physical comfort and sexual health, making proactive care essential.
Menopause and Sexual Health
Impact on Libido, Comfort, and Intimacy
Vaginal changes during menopause can directly influence sexual desire and satisfaction. Dryness and tissue thinning may cause discomfort or pain during intercourse, reducing libido and creating anxiety around intimacy.
Strategies to maintain sexual wellness include:
-
Use non-hormonal internal and external moisturizers for lubrication.
-
Focusing on foreplay and communication with partners to increase comfort.
-
Maintaining overall vaginal health through hydration, diet, and gentle hygiene.
Non-Hormonal Strategies for Maintaining Vaginal Health
Lifestyle Approaches That Support Comfort and Hydration
Even without hormone therapy, several strategies can help maintain vaginal tissue health:
-
Hydration: Adequate water intake supports natural mucosal lubrication.
-
Nutrition: Omega-3 fatty acids, vitamins C and E, zinc, and amino acids nourish vaginal tissues from within.
-
Gentle Hygiene: Avoid harsh soaps, scented products, and douching that disrupt the vaginal environment.
-
Breathable Clothing: Cotton underwear and loose-fitting clothing reduce friction and irritation.
-
Exercise: Pelvic floor exercises enhance blood flow and tissue elasticity, contributing to comfort and sexual health.
When to Seek Medical Advice
Signs You Should Consult a Gynecologist
While lifestyle adjustments and non-hormonal strategies can improve postmenopausal vaginal health, it’s important to recognize when professional evaluation is necessary. You should consult a gynecologist if you experience:
-
Persistent vaginal dryness or discomfort: Ongoing dryness that causes irritation, itching, or pain during daily activities may indicate underlying issues requiring medical attention.
-
Pain or difficulty during sexual activity: Burning, discomfort, or pain during intercourse should not be ignored, as it can affect both physical and emotional well-being.
-
Recurrent infections or unusual discharge: Frequent urinary or vaginal infections, or changes in the color, odor, or consistency of discharge, may signal imbalances or other health concerns.
-
Unexpected bleeding: Any vaginal bleeding not related to menstruation warrants immediate evaluation to rule out serious conditions.
What to Expect During a Gynecological Evaluation
A gynecologist may recommend:
-
Physical examination: Assessment of the vaginal and vulvar tissues to check for thinning, irritation, or signs of infection.
-
pH testing and cultures: To detect bacterial or yeast infections that could worsen dryness and discomfort.
-
Hormonal assessment: Measuring estrogen or other hormone levels if symptoms are severe or persistent.
-
Treatment options: Depending on the findings, treatments may include prescription vaginal moisturizers, non-hormonal supplements, topical estrogen therapies, or other individualized interventions.
Early consultation not only ensures accurate diagnosis and treatment but also prevents long-term tissue damage, preserves vaginal elasticity, and improves overall comfort and sexual health.
Frequently Asked Questions
How does menopause affect vaginal lubrication?
Declining estrogen levels reduce natural moisture, leading to dryness and increased friction during sexual activity.
Can vaginal tissue recover after menopause?
While tissue thinning may be permanent, hydration, supplements, and gentle care can improve comfort, elasticity, and lubrication.
Are hormone-free supplements effective for postmenopausal women?
Yes. Ingredients like Slippery Elm Bark, amino acids, and minerals support internal hydration and protect tissue without the need for hormones.
What lifestyle changes help maintain vaginal health after menopause?
Adequate hydration, a nutrient-rich diet, pelvic floor exercises, breathable clothing, and gentle hygiene all contribute to long-term vaginal health.
Is vaginal dryness inevitable during menopause?
Not necessarily. While many women experience dryness, preventive strategies and proper care can minimize symptoms.
When should I consider medical treatments for postmenopausal vaginal changes?
Persistent dryness, pain, infections, or bleeding should prompt consultation with a gynecologist for evaluation and treatment options.
Prioritize Vaginal Health During and After Menopause
Menopause is a natural transition, but its effects on vaginal health can significantly impact comfort and quality of life. Understanding the role of estrogen, recognizing common changes, and adopting non-hormonal strategies are key to maintaining vaginal health and sexual wellness.
Preventive care—through hydration, nutrition, gentle hygiene, internal and external moisturizers, and targeted supplements—can support tissue integrity, reduce discomfort, and enhance intimacy. By taking proactive steps, women can navigate menopause with confidence and preserve long-term vaginal health.
Share your experiences, explore non-hormonal solutions like internal hydration supplements, and consult your gynecologist for personalized guidance. Your vaginal health deserves consistent attention and care.